Introduction:
Iran’s Primary Health Care System is Excellent.
In the past three decades, the Islamic Republic of Iran has adopted a policy aimed at more strongly addressing the needs of its population, and substantial progress has been achieved both in the social and economic sectors. Since the revolution of 1979, a Primary Health Care network has been established throughout the country. In rural areas, each village or group of villages contains a Rural Health House, staffed by trained “Behvarz”.

These Rural Health Houses, which constitute the basic building blocks for Iran’s health network, are the health system’s first point of contact with the community in rural areas.
In addition, Rural Health Centers were put in place. They include a physician, a health technician and an administrator, and deal with more complex health problems.
In urban areas, similarly distributed urban health posts and Health Centers have been established. The whole network is managed and administered through District Health Centers, answerable to the Ministry of Health and Medical Education. The universities of medical sciences, of which one exists in each province, play an important role in medical education and in the provision of health services. The Chancellor of the university as executive director of the provincial health services is also in charge of all district health centers and hospitals.
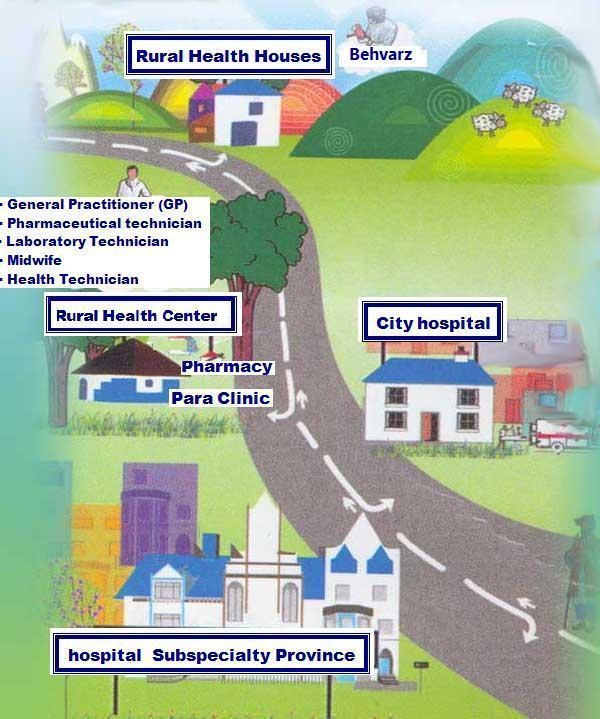
Stages of Referral system
Rural health houses are door of primary health care.
Locally sourced health workers or behvarzan from the Farsi words beh (good) and varz (skill) were originally trained to meet the basic health-care needs of people living in rural areas. A female behvarz was responsible for, among other things, child and maternal health; a male behvarz for sanitation and environmental projects. Both worked out of the health house, a rural medical post and the most basic unit of service delivery in the country’s health-care plan.
The health houses refer patients to rural health centres which cover people, and have up to two physicians and several health technicians. These centres are responsible for active and emergency case management, supporting the Rural health houses, and supervising both the health technicians and the behvarzan or community health workers.
Community health workers are often from the village they serve, their appointment confirmed by the local rural council. Their efforts have not gone unnoticed.
The Rural health workers are well familiar with the culture and traditions and that is a big advantage.
these community workers had made a significant contribution to the sharp decline in mortality rates in the past three decades, helping to reduce deaths among infants and pregnant women, and curbing contagious diseases.
the behvarzan are the axis of the village. “A community health worker is from the people and has their approval. These workers regularly supervise people’s health.”
Indeed, community health workers often have an impressive knowledge of their patients’ case histories. Log books on each household are kept at the health house. These contain the name, gender and age of all family members, sanitation conditions of the household, history of pregnancies, details of care for those aged under-five and dental-care records.
Among their duties, female community health workers are responsible for vaccinations, registrations and administering medicines. A male community health worker is charged with activities mainly outside the health house, such as making follow-up visits to patients and identifying them in surrounding villages.
plus two years of theoretical and practical training before being awarded a certificate to be allowed to practice. “Even after their graduation, the behvarzan are subject to regular monitoring and distance-learning,” Motlaq says.
the practice of keeping the “vital horoscope” – a circular chart resembling a horoscope and displaying extensive details of births, deaths and family-planning activities – is central to the health houses’ functions and provides crucial data to higher levels of the network and the Ministry of Health about the Rural health houses’ activities.
Health houses serve as the powerful arm of rural health-care centres. They did well when the main issue in the country was to contain contagious diseases. They are doing the same now chronic diseases like diabetes and hypertension, and also in improving nutrition, the control of iodine disorders, iron-deficiency anaemia and fluoride treatment.
the strengths of the Iranian primary health care system are that health houses are highly efficient compared to other health-care service-providing units (such as ambulatory and hospital services), that the primary health care system provides an effective education system for community health workers, it standardizes services and is effective also because of the community health workers’ close links with the villages in which they work.
a physician who visits the village every week.
the people come to the Rural health house for general consultations, to have their blood pressure checked, to be treated for diabetes, or for minor ailments such as the common cold.
behvarzan visited village schools once a week and tell the schoolchildren how to keep their hair, nails, mouths and teeth clean.
Resources:
http://www.unicef.org/iran/
http://www.who.int/bulletin/volumes/86/8/08-030808/en/index.html